Care Coordinators play an important role within a PCN to proactively identify and work with people, including the frail/elderly and those with long-term conditions, to provide coordination and navigation of care and support across health and care services. Care Coordinators could potentially provide extra time, capacity, and expertise to support patients in preparing for or in following-up clinical conversations they have with primary care professionals. They will work closely with the GPs and other primary care professionals within the PCN to identify and manage a caseload of identified patients, making sure that appropriate support is made available to them and their carer’s and ensuring that their changing needs are addressed. This is achieved by bringing together all the information about a person’s identified care and support needs and exploring options to meet these within a single personalised care and support plan, based on what matters to the person.
Workforce Development Framework
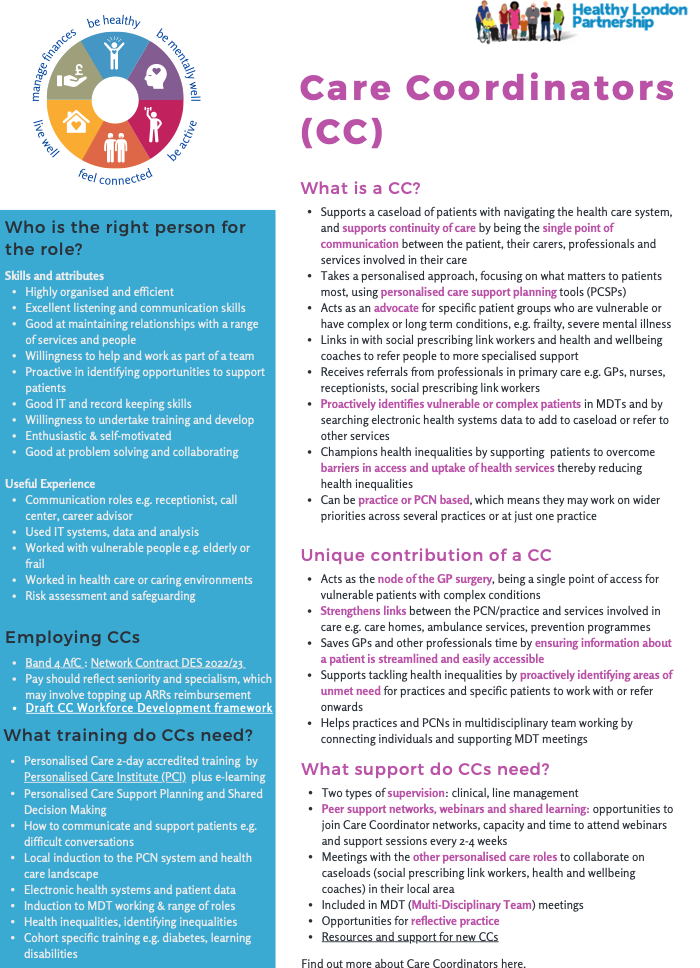
Meet our care coordinator – working alongside GPs to meet patients’ healthcare needs.
Click HERE for the Recruitment Pack
Click HERE for the Welcome Pack
| Key roles and responsibilities | Education and training requirements |
Recommended minimum supervision |
|
Enrolled in, undertaking or qualified from appropriate two-day care co-ordination training as accredited by the Personalised Care Institute
Accredited elearning completed in personalised care and support planning and shared decision making. |
A named first point of contact in the PCN (including GP). Monthly supervision can be provided by an appropriate member of the MDT including an advanced practitioner.
Further guidance on supervision, education and training can be found in the workforce development framework for care co-ordinators. |
Training/Development
Click HERE for the Minimum Training Standards & Recommended Additional Training
Care Coordinators require a strong foundation in enabling and communication skills as set out in the core Curriculum for Personalised Care. These can be achieved via a two day health coaching skills course and additional training as guided by Health Education England. Care coordinators should also access statuary and mandatory training, including but not limited to:
- Principles of information governance, accountability and clinical governance
- Maintenance of accurate and relevant records of agreed care and support needs
- Identify when it is appropriate to share information with carers and do so
- The professional and legal aspects of consent, capacity, and safeguarding
Care Coordinators should be familiar with the six components of the universal model for personalised care with a specific focus on:
- Support for self-management
- Personalised care and support planning
- Shared decision making
- Social prescribing
- Personal Health Budgets
Benefits to patients
- The patient’s go-to person if their needs change or if something goes wrong with service delivery – The care coordinator ensures that there are no gaps in the patient’s service provision – Many elderly and disabled people with highly complex needs struggle to coordinate with all the relevant services directly on their own – Improved patient education and understanding – Better health outcomes – Patients can eliminate unnecessary appointments, procedures and tests – Patients feel more empowered and actively engaged in their treatment
Benefits to PCN’s
- Ensuring seamless service provision significantly decreases the risk of the patient deteriorating and thereby reduces the overall cost of care and the likelihood that additional interventions will be needed in future. By identifying high-risk patient populations before they incur costlier medical intervention, employers can begin to reduce both practice expenses and total NHS costs – Employers can gain access to additional data that can reveal practice population health levels and risks – Care coordinators glean information about patients’ treatment histories, medication adherence, new symptoms and management of chronic conditions.
Benefits to the wider NHS
- Ensuring seamless service provision significantly decreases the risk of the patient deteriorating and thereby reduces the overall cost of care and the likelihood that additional interventions will be needed in future – By identifying high-risk patient populations before they incur costlier medical intervention, employers can begin to reduce both practice expenses and total NHS costs – Employers can gain access to additional data that can reveal practice population health levels and risks – Care coordinators glean information about patients’ treatment histories, medication adherence, new symptoms and management of chronic condition.
|
REGIONAL SUPPORT UPDATE: Our last peer support happened on Monday, we are currently planning our future offer, and some ideas are on slide 13 here. An email around the changes to support is attached. Resources and communications We have compiled all the resources, trainings and useful links into one open source google doc here! Please use this as your first port of call, we will still be here to answer any over email queries or calls for help. From next month, we’ll be sharing one monthly newsletter for all Care Coordinators, Health and Wellbeing Coaches and Social Prescribing Link Workers, you may be asked to opt into receiving this! So please watch out for this request. Care Coordinator Survey Thank you to all who completed the survey! A summary is on slide 12 here. A full breakdown of the results is here! Please do share with your managers. |
MAR PEER SUPPORT:
This is our last peer support session, whilst we plan our ongoing offer, communications about this change is attached. Thank you for all who came to the session!
During this session we covered:
- Primary care structures – sharing how the system works, what key players do in different parts of the system, what changes are happening
- Updates from the survey and regional support offer (getting feedback on potential offer)
- Closing the support – final reflections and thoughts
FEB PEER SUPPORT:
JAN PEER SUPPORT: Using EMIS in your Care Coordinator role: population searches, tips and hints
We had Nadine, a GP in Barnet run an interactive session on using EMIS for population searches.
The slides are attached. Please get in touch if you have any questions!
- SMART goal setting – Six Step Process For Setting SMART Goals – PLI (professionalleadershipinstitute.com)
- TGROW coaching model – to use when goal setting for yourself and patients classic Coaching Models – GROW, RE-GROW and T-Grow (instituteofclinicalhypnosis.com)
- Hub of Hope – search to find local mental health support
- Samaritans
- Mind
- Good thinking – mental health online platform for Londoners
- Free course – Level 2 mental health first aid training
Leadership development courses by NHS Leadership academy
A wealth of E-learnings to support your leadership, including coaching, managing people, stress management, unconscious bias, by the NHS leadership academy.
New Free Online Course – Introduction to Leadership for Personalised Care
This 3-week online course is free, easy to access and open to anyone who wants to find out more about leading a person-centred approach. Enrolment is now open and can be accessed here
Access One-Off Coaching Sessions (Express Coaching)
45 minute online coaching for NHS staff, please see here.
- Webinar recordings for understanding PCSPs and evidencing their outcomes
- New Core20PLUS5 (health inequalities) e-learning modules : Five new e-learning modules have been launched to support systems in the implementation of Core2PLUS5
- Five new massive free open online courses (MOOCs) are now available to help health and care staff improve their knowledge skills and understanding of public health research. Find out more here.
- Cancer awareness training programme by Cancer Research UK – it will equip people working or volunteering in communities with the skills and confidence to have conversations about cancer and health with the people they support. Part of the training will focus on helping people to understand the importance of spotting cancer early and the screening programmes available
- Mental health first aid training – free
- Free courses England
- Free shared decision making eLearning refresher to respond to changing patient expectations. (30 min) – For all roles in Primary Care
- All Our Health e-learning sessions have been developed to provide a bite-sized introduction to the wide range of topics including homelessness, inclusion health and NHS health checks. Within these sessions, you’ll find signposting to trusted sources of helpful evidence, guidance and support.
- There is a wealth of free training available related to health inequalities by fairhealth. It covers:
-
- What inclusion health groups are – some groups that you may focus on as a Care Coordinator
- Practical guide to health inequalities in primary care
- Performing a health needs assessment for your population
- Trauma informed care
- E-learnings on Future NHS.– specific conditions
- General personalised care e-learnings
RESOURCES
- Introducing the Personalised Care and Support Planning (PCSP) Framework – defining and implementing quality personalised care and support planning: NHS England recently published the draft PCSP Framework on our NHS Futures platform – please check out the resource!
- GP practices and the impact of health inequalities – CQC Podcast
- NHS England’s Public Participation Team have launched a new online course on Working with People and Communities to Improve Health Outcomes.
- Carnal Farrar have developed a mapping tool allowing users to explore potential inequalities in population and health metrics across each Integrated Care System (ICS).Try out the tool via this link.
- NHS England has developed a homelessness and rough sleeping (HRS) pathway, checklist and toolkit.
- NHSE five strategic priorities for tackling health inequalities
- Core20PLUS5 approach has been adapted for use in children and young people’s services.
- National share and learn recordings
- Social Prescribing newsletters (events, resources, SP news)
- Example of a personalised care support plan
- Mapping of support for cost of living
- Winter resilience plans for NHS
- Supporting High Frequency users through proactive personalised care – about what care coordinators can do
- Recording about CCs, HWBCs, SPLWs for people interested in applying for one of the roles
- Migrant Londoners Hub – information for those who have recently arrived in London.
- Secondary care case studies: These are exciting examples of Social Prescribing, Health & Wellbeing Coaching and Care Navigation supporting secondary care patients.
- Training hubs supporting personalised care roles case studies
- Film: how the non clinical ARRs roles are supporting patients in primary care – GP practice in Merton
- Tackling Health Inequalities through the personalised care ARRS roles Case Studies:
-
- Reducing Health Inequalities: deprived areas and long term conditions in Richmond
- Reducing Health Inequalities: health inclusion and homelessness in Lewisham
- Reducing Health Inequalities: health inequality strategy development in Sutton
- Reducing Health Inequalities: long Covid-19 clinics in Merton
- Reducing Health Inequalities: supporting refugees and migrants in Croydon.
- Please see this recording of the session for new Care Coordinators and share with your colleagues. It explains what the Care Coordinator role is, the value of it in primary care, what support there is as well as work examples from two care coordinators in Lewisham.
- We have a designated webpage for those that are newer in the role, where the video is hosted.
- There is also a drop in session in soon for care coordinators to ask us any questions they like – we will share this shortly.
- Personalised care collaborative: wealth of resources about personalised care, co-production, PHBs, shared decision making, choice and events.
- Primary care workforce: find out about the training hubs, wider primary care team, MDT guidance
- PCN development support: find out about ARRS, PCN development, delivery support (flu vaccines, early cancer diag, enhanced health in care homes, NHS digital weight management prog)
- Social prescribing platform: resources for social prescribing, community engagement, guides and tools to working with patients
Differences between Care Coordinator and Social Prescriber roles
These are general guidelines regarding the roles and differences between them. There may be local variations developed due to service provision and local PCN needs.
Care Coordinators
Care Coordination is a long term, integrated, evidence based programme centred around supporting people with disabilities, mental health needs, older people and their families/carers, by working together with people to help them:
- build and pursue their personal vision for a good life,
- stay strong, safe and connected as contributing citizens,
- find practical, non-service solutions to problems wherever possible,
- build more welcoming, inclusive and supportive communities.
Where local area coordination already exists in an area, it can complement social prescribing by supporting particular cohorts of people for the longer term and building community capacity and connections.
Social Prescriber Link Worker
Social prescribing links patients with non-medical support to improve their physical and mental wellbeing. Link workers give people time and focus on what matters to the person as identified through shared decision- making or personalised care and support planning. They connect people to community groups and agencies for practical and emotional support.
Social prescribing works for a wide range of people, including those:
- with one or more long-term conditions
- who need support with their mental health
- who are lonely or isolated
- who have complex social needs which affect their wellbeing.
SPLW have an important role to play in the community too. Working closely with local partners, they can identify and address gaps in voluntary and community sector as well as helping to make groups sustainable. The roles refer back to each other to improve patient resilience and build the wider team around the patient.